Dental Products Report | October 14, 2020
When the American Dental Association asked dental offices to temporarily close, except for emergencies, on March 16, 2020, little was known about the relationship between oral hygiene and the severity of COVID-19 infections. Since that time, new research is showing that poor oral hygiene can directly affect how patients are able to fight off the disease. The short-term lack of access to preventative dental care, especially in minority populations, now underscores the risk factors that can accompany poor oral hygiene, including diabetes, hypertension, obesity and cardiovascular disease.
A recent article published in the British Dental Journal in June 2020 reflects that relationship in a very relevant and urgent way. It concludes that poor oral hygiene may be connected to serious COVID-19 complications due to high levels of harmful oral bacteria.1 The authors explored the connection between high bacterial load in the mouth and post-viral complications, and how improving oral health may reduce the risk of complications from COVID-19. They concluded that the development, severity, and risk of complications following a COVID-19 infection depend on a number of host and viral infections.
The four main co-morbidities related to COVID-19 are also associated with altered oral biofilms and periodontal disease. In addition, an article published in Dental Research and Management detailed the close relationship between a number of systemic conditions that are all most likely initiated by one single oral pathogen strain.2 The prevention of these prevalent systemic illnesses needs to be started at the earliest possible point, with intervention starting with good Oral Maternal-Fetal health.3
COVID-19 affects people in different ways, with patients exhibiting a range of symptoms and severity. So why do some people suffer more severely? Its become clear that bacterial superinfections are common in patients suffering from a severe case of COVID-19. Over 80% of COVID-19 patients in ICUs exhibited an exceptionally high bacterial load, with more than 50% of deaths exhibiting bacterial superinfections.
While COVID-19 has a viral origin, its suspected that in severe cases, complications such as pneumonia and acute respiratory distress (ARDS) may be caused by bacterial superinfections. And those bacteria may originate in the mouth. In addition, SAR-CoV-2 has a significant salivary level, providing for testing with salivary sampling. The oral cavity, via saliva and plaque, is strongly felt to be significant in the modes of transmission with COVID-19.
How bacteria travel from the mouth to the lungs
The oral microbiome is considered a gateway microbiome. Our human-specific oral microbial species have all evolved with the host to help protect the host and to also process the nutritional intake of the host. The oral bacteria, yeasts, viruses, archaea number in the thousands of strains, and rapidly adapt to dietary influences, allowing for homo sapiens to change and survive. Significant dietary changes in our developmental history, with the massive increase in carbohydrates, encouraged the expansion of pathogenic strains that injure the human host, even suppressing the hosts immune responses. Maintenance of a healthy oral microbiome is therefore essential.
Micro-organisms that colonize the mouth propagate via the saliva. The pathogenic bacteria or viruses within the saliva can then be aspirated into the lower respiratory tract and cause or aggravate an infection. Periodontitis and decay are the two most common oral diseases associated with an imbalance of pathological bacteria in the mouth. This imbalance is a Dysbiosis, whereas the increase in pathogens follows the decrease in competing probiotic bacteria and the strain shifting of commensals into co-pathogens. This illustration from the British Dental Journal shows how that works.
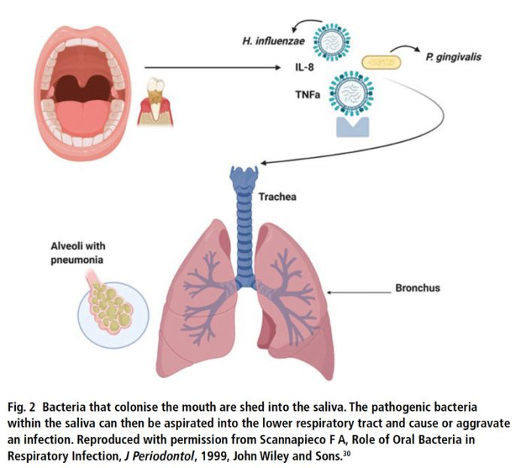 Image by British Dental Journal
Image by British Dental JournalOral health probiotics
Oral care probiotics seem to be relatively new to the dental industry and are often confused with traditional probiotics, which are designed to improve gut health. However, oral-care probiotic research is more than 35 years old and the best products have been around for more than 10 years. There are scientific distinctions that can help dentists prescribe and consumers choose the best product for their patients. Those that support throat health only provide minimal support to the health of teeth and gums, while those oral-care probiotics that use gum and tooth specific strains provide the best overall support and benefits to both periodontal and tooth health and have the longest research behind them.
Generally speaking, oral care probiotics are live bacteria that are identical to the beneficial microorganisms found naturally in the oral biome. The addition of oral care probiotics to an oral care regimen can restore the natural balance of the oral biome by repopulating beneficial bacteria, which can be depleted by diet, stress, medication, illness, or other factors.
Specifically, only oral care probiotics that include bacteria Streptococcus oralis KJ3, Streptococcus uberis KJ2, and Streptococcus rattus H145, support teeth and gums, the inherent source of these strains. These products can be seen as a first line defense against pathogens coming into the mouth. While all patients will see benefits, for those with periodontal disease, caries, and other oral care concerns, oral care probiotics are an effective adjunct to extend treatment benefits.
One key takeaway from this article is that, with COVID-19 and other viral diseases, inadequate oral hygiene can increase the risk of inter-bacterial exchanges between the lungs and the mouth, increasing the risk of respiratory infections and potentially post-viral bacterial complications.4
Good oral hygiene has been recognized as a means to prevent airway infections in patients, especially in those over the age of 70. In fact, studies show that improved oral care can significantly reduce the incidence of ventilator-associated pneumonia in ICU patients.
The other key takeaway from the articles authors is that improved oral hygiene may play a part in reducing the risk of complications. The authors write, We recommend that oral hygiene be maintained, if not improved, during a SARS-CoV-2 infection in order to reduce the bacterial load in the mouth and the potential risk of a bacterial superinfection.1
In addition to diligent home care, adding oral care probiotics to the daily regime can also help reduce harmful bacteria in the mouth. According to my recent peer-reviewed study in the Journal of Clinical Pediatric Dentistry, (oral care) probiotics significantly reduced the caries rate of high caries prone pediatric subjects without any reported side effects.5 The article continues, Indeed, probiotics simply reduce the pathogens that modern, high sugar diets, feed. While the study was conducted on children over a three-year time period, the findings can be extrapolated to adults, who may also benefit from taking oral care probiotics to reduce the bacterial load in the mouth.
Preventive care continues to be a problem during the pandemic, as patients may be fearful of returning to their dentists. Home care has never been so important. Our patient protocol includes testing, treating, and repopulating the beneficial bacteria in the mouth, says Lora Hooper, BS, RDH, FDA Dental Hygiene, part of the oral care team at the Heart Attack and Stroke Prevention Center of Central Ohio. I have seen a dramatic improvement in oral health in patients using oral care probiotics. The practice is run jointly by a dentist and cardiologist, who unify oral and systemic care for all patients.
As the search for COVID-19 treatments and vaccines continues, dentists and hygienists can help patients stay healthy with good communication and education. Oral health is a key factor in helping fight the pandemic. Were all in this together.

